Abstract
Background
In patients with follicular lymphoma (FL) the clinical international prognostic index FLIPI is well established, but recently the impact of a number of gene mutations was evaluated. The m7-FLIPI prognostic model, derived from the FLIPI score combined with ECOG and the mutational status of seven specific genes, was shown to stratify FL patients into "low-risk" and "high-risk" with respect to 5-year failure-free survival after first-line immunochemotherapy (R-CHOP or R-CVP) (Pastore, Lancet Oncol 2015). The Nordic Lymphoma Group (NLG) performed two trials (accrual 1998-1999 and 2002-2008, respectively) including a total of 439 patients with symptomatic/progressing indolent B-cell lymphoma (79% FL) randomized 1:1 to treatment with single rituximab or rituximab plus interferon-α2a (Kimby, Leuk Lymphoma 2008, 2015). A follow-up study after 10 years found 36% still chemotherapy-free (Lockmer, JCO 2018).
Aim: As part of a long-term follow-up of we aimed to investigate whether the m7-FLIPI prognostic model could be validated in a FL patient cohort treated with first-line-immunotherapy only.
Methods
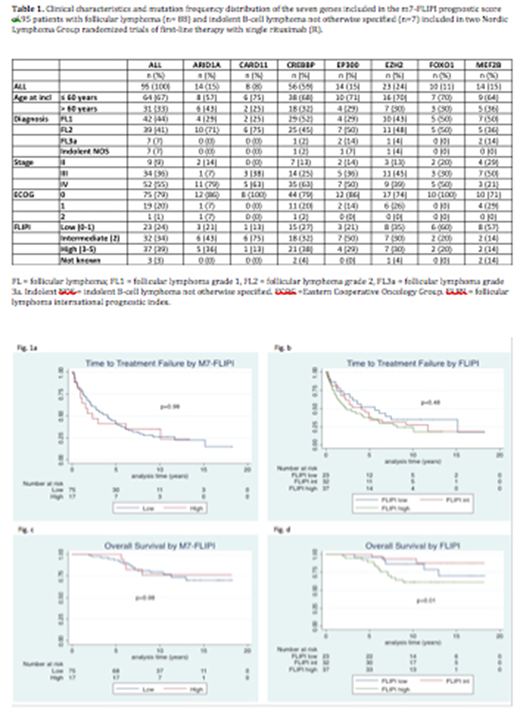
Fresh-frozen diagnostic lymph node biopsies with sufficient material for gene sequencing were available from 88 patients with verified FL grades 1-3a and 7 patients with indolent B-cell lymphoma not otherwise specified. A targeted Lymphochip panel including the seven genes of the m7-FLIPI, EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP and CARD11, was used. Clinical data were retrieved from the databases of the two trials and from follow-up medical records. Variables assessed included all post-trial therapies, the last dates of follow-up and causes of death. The m7-FLIPI score was calculated according to the published sum of predictor algorithm with respect to high-risk FLIPI, ECOG >1 and occurrence of non-silent mutations. Time to treatment failure (TTF), the primary endpoint, was defined as the interval between start of trial therapy and either initiation of new lymphoma therapy due to relapse or intolerance, or death from any cause. TTF was chosen rather than the date of stable or progressive disease described in the Pastore report, as the date of new therapy is less affected by assessment frequency and quality. The Pastore cut-off score of ≥ 0.84 for discrimination between the m7-FLIPI high- vs low-risk group was applied. TTF and overall survival (OS) were estimated with the Kaplan-Meier method and the log-rank test applied for comparison between risk groups.
Results
Mutational status was obtained from 95 patients, four of them with two biopsies each. In two of the doublets mutations differed between samples in which case the earliest dated samples was chosen for risk analyses. Three patients (two FL) could not be risk-stratified according to the m7-FLIPI score due to missing clinical information. Patient characteristics and gene mutations are shown in Table 1. The mutation frequency distribution was broadly similar to the Pastore report cohorts, mutations in the epigenetic modifier CREBBP by far the most common. With a median follow-up after randomization of 10.6 (range 0.6-18.3) years, 72 (76%) patients were alive. Of all, 28% had never required any new therapy, and 39% had not required any chemotherapy. For 13 out of 23 patients the cause of death was lymphoma-related i.e. due to progression of disease or complications of therapy. No difference in TTF nor OS was found between the m7-FLIPI high- vs low-risk group (fig 1a-b), but in the high-risk FLIPI group OS was shorter (fig 1d). Mutation in the EZH2 gene, coding for the catalytic subunit of a histone methyltransferase, was associated with longer TTF (p=0.04) also within FLIPI risk groups but not with OS (p=0.63).
Conclusion
The m7-FLIPI prognostic clinicogenetic model was not valid in our cohort with FL patients treated with only immunotherapy. Mutation in the gene EZH2 was associated with longer TTF and high-risk FLIPI with shorter OS.
Wahlin:Gilead: Consultancy, Honoraria, Research Funding; Roche: Research Funding. Kimby:AbbVie: Membership on an entity's Board of Directors or advisory committees; Gilead: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees; Roche: Honoraria; Roche: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal